Newly published study:
http://www.journalacs.org/article/S1072-7515(14)00927-2/fulltext
Article Outline
- Introduction
- Methods
- Results
- Conclusions
Jump to SectionIntroductionMethodsResultsConclusions
Introduction
To compare mid-term results of LGB and single-anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S), a modified one-loop duodenal switch.
Jump to SectionIntroductionMethodsResultsConclusions
Methods
We performed a prospective comparison of 215 morbidly obese patients submitted to LGB (n= 115) or SADI-S (n= 89) between July 2009 and December 2012.
Jump to SectionIntroductionMethodsResultsConclusions
Results
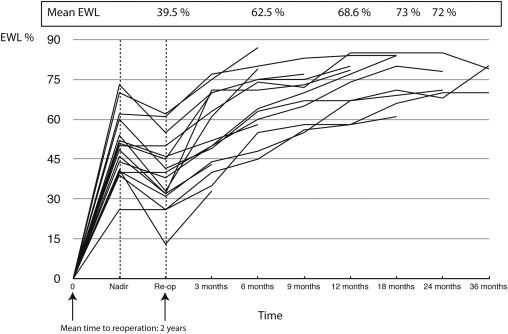
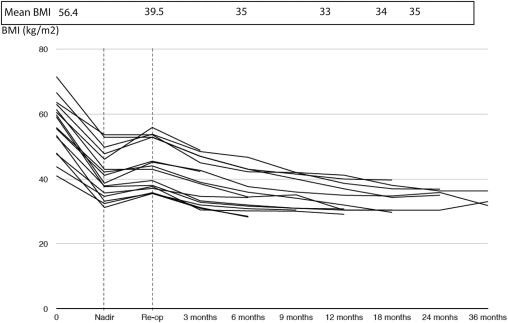
The groups were similar in terms of age and sex. The SADI-S group had significantly higher Body Mass Index (BMI) (42.37 vs 45.34, p = 0.001) and more comorbidities (hypertension, type 2 diabetes and obstructive sleep apnea). Early complications occurred more often in LGB than in SADI-S (20% vs 8.9%; P = <0.05).The difference in severe complications did not reach statistical significance (5% for LGB vs 2% for SADI-S; P = 0.66).The mean % of Excess weight loss (EWL) for both groups during the first year after the surgery was similar. The SADI-S group presented a higher and maintained EWL at 18 months (80 ± 21.43 vs 95.47 ± 20.4; P = 0.001), 24 months (77.68 ± 19.39 vs 93.67 ± 23.14; P = 0.001) and 36 months (75.84 ± 27.88 vs 91.33 ± 29.07; P = 0.03).The SADI-S group presented more remission of hypertension (27% 39 % p 0.002) and type 2 diabetes (67% vs 85%, p<0.005).
Jump to SectionIntroductionMethodsResultsConclusions
Conclusions
Both techniques carry out a low rate of postoperative complications. Both procedures were efficient regarding weight loss and improvement of comorbidities. In the mid-term, SADI-S, a modified duodenal switch, offers a better weight loss and a better metabolic response than LGB.