I might have contributed to this ... it is very damaging, regressive and what Anthem BC does in CA, often gets promulgated to other BC franchisee, and other insurance companies.
~~~~~~~~~~
http://blog.dssurgery.com/2015/01/weight-loss-surgery-coverage-changes.html
Weight loss Surgery Coverage Changes
Weight loss surgical procedures have been proven to be the only viable option for sustained weight loss when compared to all other modalities, including diet, exercise, behaviors modifications, appetite suppressant, and other less scientific approaches.
Different weight loss procedures have had varying degree of success as measured with resolution of the co-morbidities and long term weight loss.
In December of 2014, Blue Cross of California notified the providers of a number of changes in their coverage will be taking place.
One such specific modification in policy involves primary and revision weight loss surgery.
These policy changes have significant practical implications for those seeking surgical treatment for morbid obesity and associated co-morbidities.
First of all, they create a road block for those patients who are not able to provide documentation for the "...6 continuous months, in the 2 years prior to surgery, to enable both behavioral changes and adequate assessment of anticipated postoperative dietary maintenance." It also places the responsibility on the surgeon by requiring that compliance with these requiremens are ".... fully appraised and documented by the physician requesting authorization for surgery."
The practical implication of this is much longer wait between the first office visit with a surgeon and the ability to obtain authorization unless a patient comes in with 6 months’ worth of documentation. The impropriety of such medically unsubstantiated requirements, including the unacceptable and harmful effect of delay or denial on access to medically necessary treatment, was addressed by the ASMBS in the March 2011 position statement on Preoperative Supervised Weight Loss Requirements (http://asmbs.org/resources/preoperative-supervised-weight-loss-requirements). These new requirements are inconsistent with the ASMBS Position Statement and should be vigorously opposed.
The second and in my opinion more restrictive and significant change is for revision procedures. It indicates that any patients in need of a medically necessary revision surgery, must meet the criteria for initial weight loss surgery. This can dramatically limit access to revision surgery for those who are having complications, e.g., of the Adjustable Gastric banding procedures (because they are unable to eat, having constant nausea and vomiting, abdominal pain etc.) or gastric bypass (dumping syndrome, solid intolerance, etc.) but who do not meet the weight criteria or have documentation for 6 months of “ … participation in a non -surgical weight loss ..." since they were not trying to lose weight.
This should also concern those who have or perform the duodenal switch as a staged procedure, where the sleeve is done as the first step, to be followed by the completion of duodenal switch operation at a later time. Although I am generally against a staged approach to the duodenal switch operation, this policy change introduces unnecessary and even insurmountable hurdles for those patients for whom this approach is deemed medically necessary.
For all those who are not in California, please note that a lot of policies do start here and propagate to the rest of the country. I would propose that everyone take time to contact their state health insurance providers regulatory agency and voice their opposition to the proposed changes.
The state regulatory agencies are located here. (http://www.dsfacts.com/image-files-new/agencies-by-state.pdf)
~~~~~~~~~~
http://blog.dssurgery.com/2015/01/weight-loss-surgery-coverage-changes.html
Weight loss Surgery Coverage Changes
Weight loss surgical procedures have been proven to be the only viable option for sustained weight loss when compared to all other modalities, including diet, exercise, behaviors modifications, appetite suppressant, and other less scientific approaches.
Different weight loss procedures have had varying degree of success as measured with resolution of the co-morbidities and long term weight loss.
In December of 2014, Blue Cross of California notified the providers of a number of changes in their coverage will be taking place.
One such specific modification in policy involves primary and revision weight loss surgery.
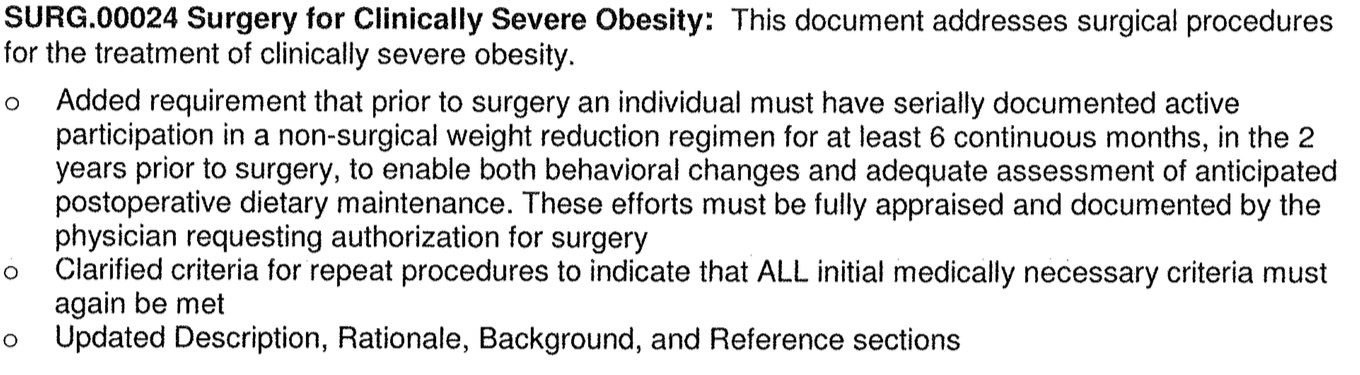
These policy changes have significant practical implications for those seeking surgical treatment for morbid obesity and associated co-morbidities.
First of all, they create a road block for those patients who are not able to provide documentation for the "...6 continuous months, in the 2 years prior to surgery, to enable both behavioral changes and adequate assessment of anticipated postoperative dietary maintenance." It also places the responsibility on the surgeon by requiring that compliance with these requiremens are ".... fully appraised and documented by the physician requesting authorization for surgery."
The practical implication of this is much longer wait between the first office visit with a surgeon and the ability to obtain authorization unless a patient comes in with 6 months’ worth of documentation. The impropriety of such medically unsubstantiated requirements, including the unacceptable and harmful effect of delay or denial on access to medically necessary treatment, was addressed by the ASMBS in the March 2011 position statement on Preoperative Supervised Weight Loss Requirements (http://asmbs.org/resources/preoperative-supervised-weight-loss-requirements). These new requirements are inconsistent with the ASMBS Position Statement and should be vigorously opposed.
The second and in my opinion more restrictive and significant change is for revision procedures. It indicates that any patients in need of a medically necessary revision surgery, must meet the criteria for initial weight loss surgery. This can dramatically limit access to revision surgery for those who are having complications, e.g., of the Adjustable Gastric banding procedures (because they are unable to eat, having constant nausea and vomiting, abdominal pain etc.) or gastric bypass (dumping syndrome, solid intolerance, etc.) but who do not meet the weight criteria or have documentation for 6 months of “ … participation in a non -surgical weight loss ..." since they were not trying to lose weight.
This should also concern those who have or perform the duodenal switch as a staged procedure, where the sleeve is done as the first step, to be followed by the completion of duodenal switch operation at a later time. Although I am generally against a staged approach to the duodenal switch operation, this policy change introduces unnecessary and even insurmountable hurdles for those patients for whom this approach is deemed medically necessary.
For all those who are not in California, please note that a lot of policies do start here and propagate to the rest of the country. I would propose that everyone take time to contact their state health insurance providers regulatory agency and voice their opposition to the proposed changes.
The state regulatory agencies are located here. (http://www.dsfacts.com/image-files-new/agencies-by-state.pdf)

